Connect With Us
Blog

Understanding Foot Changes During Pregnancy

Pregnancy is a transformative journey marked by numerous bodily changes, including those affecting the feet. As the body undergoes hormonal shifts and weight gain, the feet bear the brunt of these transformations, often resulting in the development of various foot conditions. Swelling, or edema, is a common occurrence due to fluid retention, causing the feet to appear puffy and uncomfortable. Additionally, the increased pressure on the arches may lead to the onset or exacerbation of conditions such as plantar fasciitis or flat feet. Hormonal changes can also impact ligaments and joints, potentially causing instability and discomfort in the ankles and feet. To mitigate these issues, pregnant individuals are advised to wear supportive footwear, elevate their feet when possible, and engage in gentle exercises to improve circulation and alleviate swelling. If you have developed foot conditions during your pregnancy, it is suggested that you schedule an appointment with a podiatrist who can guide you toward finding relief.
Pregnant women with swollen feet can be treated with a variety of different methods that are readily available. For more information about other cures for swollen feet during pregnancy, consult with Emmanuel Bustos, DPM from New York. Our doctor will attend to all of your foot and ankle needs.
What Foot Problems Can Arise During Pregnancy?
One problem that can occur is overpronation, which occurs when the arch of the foot flattens and tends to roll inward. This can cause pain and discomfort in your heels while you’re walking or even just standing up, trying to support your baby.
Another problem is edema, or swelling in the extremities. This often affects the feet during pregnancy but tends to occur in the later stages.
How Can I Keep My Feet Healthy During Pregnancy?
- Wearing orthotics can provide extra support for the feet and help distribute weight evenly
- Minimize the amount of time spent walking barefoot
- Wear shoes with good arch support
- Wear shoes that allow for good circulation to the feet
- Elevate feet if you experience swelling
- Massage your feet
- Get regular, light exercise, such as walking, to promote blood circulation to the feet
If you have any questions please feel free to contact our office located in New York, NY . We offer the newest diagnostic and treatment technologies for all your foot and ankle needs.
Pregnancy and Foot Health
Many pregnant women complain about foot pain while they are expecting. Foot pain can primarily be caused by weight gain and hormonal changes taking place in the body. By understanding how pregnancy impacts the health of a woman's feet, a pregnant woman can take action to keep her feet as healthy and comfortable as possible.
Because a woman's weight changes during pregnancy, more pressure is brought to bear on both the legs and the feet. This weight shift can cause two major foot problems: over-pronation, also known as flat feet, as well as edema, which is swelling of the feet. Over-pronation occurs when the arch of the foot flattens, causing the foot to roll inwards when the individual is walking, and can aggravate the plantar fascia tissues located along the bottom of the feet. If these tissues become inflamed, a pregnant woman can experience pain in the heel of the foot as well as severe foot pain while walking or standing. Swelling of the feet, or edema, often occurs in the later stages of pregnancy. It is caused by slow circulation and water retention, and may turn the feet a light purple color.
To keep feet in good health and prevent over-pronation, pregnant women should avoid walking barefoot and be sure they are wearing shoes that offer good arch support. A device known as an orthotic can be added to regular footwear in order to provide additional support for the feet during pregnancy. Any expectant mother whose feet hurt should first check to see if the shoes she is wearing are old, worn out and not offering the proper support necessary for distributing the weight of her body during pregnancy.
To treat edema of the feet, a good start is to wear quality footwear which offers support and good circulation. Keep feet elevated whenever possible by using a foot stool while seated. Stay well hydrated by drinking plenty of water to prevent water retention in the feet. Any swelling that occurs in only one foot should be examined as soon as possible by a doctor.
Good foot health during pregnancy can help expectant mothers avoid foot pain that leads to other health problems. Massaging the feet and doing regular gentle exercise like walking aids foot health by contributing to good circulation. Supportive shoes are also a good investment that will support foot health during pregnancy.
Risks Posed by Cracked Heels
 Leaving cracked heels untreated poses several risks that can affect your health. When the skin on the heels becomes excessively dry and develops calluses, it leads to deep fissures or cracks. These openings increase the risk of foot infections and leave an entry point for bacteria. Cracked heels can also lead to pain, discomfort, and difficulty walking, which may interfere with day-to-day activities. In severe cases, untreated cracked heels may result in bleeding and increase the risk of cellulitis, a serious bacterial skin infection. Foot wounds may develop when cracked heels become infected, and this is especially important to avoid for people with diabetes and the associated loss of circulation in the feet. Cracked heels may also signal underlying health issues, such as vitamin deficiencies or thyroid disorders. If you have cracked heels, it is suggested you make an appointment with a podiatrist who can treat the issue and prevent complications.
Leaving cracked heels untreated poses several risks that can affect your health. When the skin on the heels becomes excessively dry and develops calluses, it leads to deep fissures or cracks. These openings increase the risk of foot infections and leave an entry point for bacteria. Cracked heels can also lead to pain, discomfort, and difficulty walking, which may interfere with day-to-day activities. In severe cases, untreated cracked heels may result in bleeding and increase the risk of cellulitis, a serious bacterial skin infection. Foot wounds may develop when cracked heels become infected, and this is especially important to avoid for people with diabetes and the associated loss of circulation in the feet. Cracked heels may also signal underlying health issues, such as vitamin deficiencies or thyroid disorders. If you have cracked heels, it is suggested you make an appointment with a podiatrist who can treat the issue and prevent complications.
If the skin on your feet starts to crack, you may want to see a podiatrist to find treatment. If you have any concerns, contact Emmanuel Bustos, DPM from New York. Our doctor can provide the care you need to keep you pain-free and on your feet.
Cracked Heels
It is important to moisturize your cracked heels in order to prevent pain, bleeding, and infection. The reason cracked heels form is because the skin on the foot is too dry to support the immense pressure placed on them. When the foot expands, the dry skin on the foot begins to split.
Ways to Help Heal Them
- Invest in a good foot cream
- Try Using Petroleum Jelly
- Ease up on Soaps
- Drink Plenty of Water
Ways to Prevent Cracked Heels
- Moisturize After Showering
- Skip a Shower
- Keep Shower Water Lukewarm
- Don’t Scrub Your Feet
If you are unsure how to proceed in treating cracked heels, seek guidance from a podiatrist. Your doctor will help you with any questions or information you may need.
If you have any questions, please feel free to contact our office located in New York, NY . We offer the newest diagnostic and treatment technologies for all your foot care needs.
Solutions for Cracked Heels
Cracked heels may make you want to think twice about showing off your feet in warmer weather. However, cracked heels may be harmful to more than just the appearance of your feet. If deep fissures and cracks develop in your heels, they may make walking and standing painful for you. Additionally, these openings make way for germs to enter through your skin and cause infection.
There are several different causes of cracked heels. One of the most common reasons for this ailment is dry skin. This problem may make your keeps feel rough tight and itchy. Dry skin may be caused by cold air, extremely hot water, harsh soaps, and aging. Skin disorders such as eczema and psoriasis may eventually lead to dry skin. In some cases, complications may arise from cracked heels. Some of these complications are a loss of feeling in the heel, cellulitis, or a diabetic foot ulcer.
There are ways you can try to prevent getting cracked heels. One of the best ways to do so is to avoid wearing flip flops and sandals because these shoes increase your risk of drying out your feet. You should also avoid wearing shoes with a tall skinny heel, because these shoes cause your heel to expand sideways. At night, you should slather on a thick moisturizing cream on your feet and then cover them in socks to keep your feet moisturized overnight. Drinking water to stay hydrated is also a good way to ensure that your skin doesn’t become dry.
If you suffer from a severe case of cracked feet, you should make an appointment with your podiatrist to see what treatment methods are best for you.
Dealing With an Achilles Tendon Rupture

In cases of a complete tear of the Achilles tendon, surgery becomes a necessary consideration. This procedure involves carefully bringing the torn ends of the tendon together and stitching them to promote healing. While Achilles tendon repair surgery is generally safe, it's not without risks. Complications can include nerve damage, foot swelling, and issues with blood flow. Further, there's a slight risk of re-rupture, emphasizing the need for thorough post-operative care and rehabilitation. Following surgery, diligent pain management and adherence to post-operative instructions are essential for a smooth recovery. This typically includes wearing a cast or splint, elevating the leg, and gradually reintroducing activities over several months. Full recovery can take up to nine months. If you believe you have torn your Achilles tendon injury or have concerns about treatment options, it is suggested that you contact a podiatrist immediately for an exam, a diagnosis, and treatment options.
Achilles tendon injuries need immediate attention to avoid future complications. If you have any concerns, contact Emmanuel Bustos, DPM of New York. Our doctor can provide the care you need to keep you pain-free and on your feet.
What Is the Achilles Tendon?
The Achilles tendon is a tendon that connects the lower leg muscles and calf to the heel of the foot. It is the strongest tendon in the human body and is essential for making movement possible. Because this tendon is such an integral part of the body, any injuries to it can create immense difficulties and should immediately be presented to a doctor.
What Are the Symptoms of an Achilles Tendon Injury?
There are various types of injuries that can affect the Achilles tendon. The two most common injuries are Achilles tendinitis and ruptures of the tendon.
Achilles Tendinitis Symptoms
- Inflammation
- Dull to severe pain
- Increased blood flow to the tendon
- Thickening of the tendon
Rupture Symptoms
- Extreme pain and swelling in the foot
- Total immobility
Treatment and Prevention
Achilles tendon injuries are diagnosed by a thorough physical evaluation, which can include an MRI. Treatment involves rest, physical therapy, and in some cases, surgery. However, various preventative measures can be taken to avoid these injuries, such as:
- Thorough stretching of the tendon before and after exercise
- Strengthening exercises like calf raises, squats, leg curls, leg extensions, leg raises, lunges, and leg presses
If you have any questions please feel free to contact our office located in New York, NY . We offer the newest diagnostic tools and technology to treat your foot and ankle needs.
What are Achilles Tendon Injuries
The Achilles tendon is the strongest tendon in the human body. Its purpose is to connect the lower leg muscles and calf to the heel of the foot. This tendon is responsible for facilitating all types of movement, like walking and running. This tendon provides an enormous amount of mobility for the body. Any injuries inflicted to this tissue should be immediately brought up with a physician to prevent further damage.
The most common injuries that can trouble the Achilles tendon are tendon ruptures and Achilles tendinitis. Achilles tendinitis is the milder of the two injuries. It can be recognized by the following symptoms: inflammation, dull-to-severe pain, increased blood flow to the tendon, thickening of the tendon, and slower movement time. Tendinitis can be treated via several methods and is often diagnosed by an MRI.
An Achilles tendon rupture is trickier to heal, and is by far the most painful injury. It is caused by the tendon ripping or completely snapping. The results are immediate and absolutely devastating, and will render the patient immobile. If a rupture or tear occurs, operative and non-operative methods are available. Once the treatment begins, depending on the severity of the injury, recovery time for these types of issues can take up to a year.
Simple preventative measures can be taken as a means to avoid both injuries. Prior to any movement, taking a few minutes to stretch out the tendon is a great way to stimulate the tissue. Calf raises, squats, leg curls, leg extensions, leg raises, lunges, and leg presses are all suggested ways to help strengthen the lower legs and promote Achilles tendon health.
Many problems arise among athletes and people who overexert themselves while exercising. Problems can also happen among those who do not warm up properly before beginning an activity. Proper, comfortable shoes that fit correctly can also decrease tendon injuries. Some professionals also suggest that when exercising, you should make sure that the floor you are on is cushioned or has a mat. This will relieve pressure on the heels. A healthy diet will also increase tendon health.
It is very important to seek out a podiatrist if you believe you have an injury in the Achilles region. Further damage could result in severe complications that would make being mobile difficult, if not impossible.
Key Insights Into Foot Pain From Plantar Fasciitis
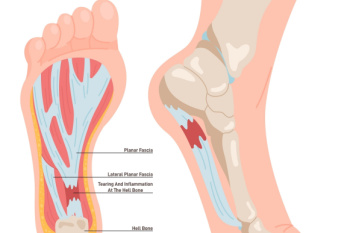
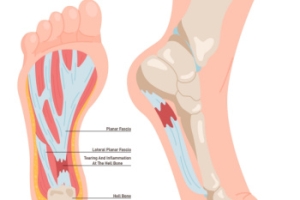
Plantar fasciitis, a common foot ailment, affects millions of individuals worldwide, causing discomfort and hindering mobility. This condition occurs when the plantar fascia, a thick band of tissue connecting the heel bone to the toes, becomes inflamed or strained. It is characterized by sharp pain at the bottom of the foot, particularly near the heel, especially noticeable during the first steps in the morning or after prolonged periods of rest. While the exact cause remains elusive, factors such as overuse, improper footwear, high-impact activities, and tight calf muscles contribute to its onset. Plantar fasciitis is prevalent among athletes, runners, and individuals who spend extended periods on their feet. Fortunately, conservative treatments like rest, stretching exercises, and orthotic inserts, can alleviate symptoms and promote healing in many cases. However, persistent cases may require medical intervention, including corticosteroid injections or surgical procedures. If you have heel pain, it is suggested that you confer with a podiatrist who can accurately diagnose and treat plantar fasciitis.
Plantar fasciitis can be very painful and inconvenient. If you are experiencing heel pain or symptoms of plantar fasciitis, contact Emmanuel Bustos, DPM from New York. Our doctor can provide the care you need to keep you pain-free and on your feet.
What Is Plantar Fasciitis?
Plantar fasciitis is the inflammation of the thick band of tissue that runs along the bottom of your foot, known as the plantar fascia, and causes mild to severe heel pain.
What Causes Plantar Fasciitis?
- Excessive running
- Non-supportive shoes
- Overpronation
- Repeated stretching and tearing of the plantar fascia
How Can It Be Treated?
- Conservative measures – anti-inflammatories, ice packs, stretching exercises, physical therapy, orthotic devices
- Shockwave therapy – sound waves are sent to the affected area to facilitate healing and are usually used for chronic cases of plantar fasciitis
- Surgery – usually only used as a last resort when all else fails. The plantar fascia can be surgically detached from the heel
While very treatable, plantar fasciitis is definitely not something that should be ignored. Especially in severe cases, speaking to your doctor right away is highly recommended to avoid complications and severe heel pain. Your podiatrist can work with you to provide the appropriate treatment options tailored to your condition.
If you have any questions please feel free to contact our office located in New York, NY . We offer the newest diagnostic and treatment technologies for all your foot and ankle needs.
Plantar Fasciitis
The plantar fascia is a connective tissue in the heel that stretches across the bottom length of your foot. Plantar fasciitis occurs when the connective tissue becomes inflamed, causing heel pain and discomfort during physical activity. Although the condition is completely treatable, traditional methods can take up to a year to start becoming effective.
Plantar fasciitis is caused by a number of everyday activities, so understanding the condition is important for managing and treating it. One of the most common causes of plantar fasciitis is excessive running, especially with improper fitting or non-supportive shoes. Too much exercise can lead to the plantar fascia being overworked and overstretched, which can cause tears in the tissue. Along with improper fitting shoes, pronation, the rolling of the feet inward, is a common cause of plantar fasciitis. If not treated properly, the plantar fascia becomes overstretched and starts to tear, causing inflammation.
Despite the common causes of plantar fasciitis, there are many different treatment options. For less severe cases, conservative home remedies include taking anti-inflammatory drugs to alleviate pain, applying ice packs to the bottom of your foot and heel, slowly stretching and exercising your feet to re-strengthen the tissue, and using orthotic devices are all ways to help manage your plantar fasciitis.
For more severe cases, shockwave therapy has become a common solution for plantar fasciitis. Shockwave therapy can effectively break up the tissue on the bottom of your foot which facilitates healing and regeneration. This fights the chronic pain caused by plantar fasciitis. Even if this doesn’t work, surgery is always a final option. Surgery on the tissue itself can be done to permanently correct the issue and stop the inflammation and pain in your heels.
No matter what the case may be, consulting your podiatrist is the first and best step to recovery. Even the slightest amount of heel pain could be the first stage of plantar fasciitis. Untreated symptoms can lead to the tearing and overstretching of tissue. Because the tearing of tissue can be compounded if it remains ignored, it can evolve into a severe case. The solution is early detection and early treatment. Talk to your podiatrist about the possibilities of plantar fasciitis if you’re experiencing heel pain.
Many Causes of Foot Arch Pain

The human foot, with its intricate network of bones, is organized into two arches, one running the length of the foot and other the width. The arches are supported by ligaments, muscles, and the plantar fascia, which runs beneath the foot. They function as a shock absorbing system during walking. Foot pain can be felt in the arches, including muscle strain, ligament sprains, fractures, poor alignment, or tightness within the foot's structures. Inflammation of the plantar fascia, often due to injury or repetitive stress, commonly leads to discomfort and restricted mobility. Symptoms of arch pain can include a dull ache in the bottom of the foot, a sign of plantar fasciitis, or specific joint tenderness or swelling, which may indicate a sprain or fracture, necessitating prompt medical attention. Conditions such as arthritis or stress fractures can also result from repetitive stress or trauma to the foot muscles or bones. A physical examination by a podiatrist, imaging tests, and gait analysis may be needed. If you are suffering from arch pain, it is suggested that you schedule an appointment with a podiatrist for treatment options.
Foot Pain
Foot pain can be extremely painful and debilitating. If you have a foot pain, consult with Emmanuel Bustos, DPM from New York. Our doctor will assess your condition and provide you with quality foot and ankle treatment.
Causes
Foot pain is a very broad condition that could be caused by one or more ailments. The most common include:
- Bunions
- Hammertoes
- Plantar Fasciitis
- Bone Spurs
- Corns
- Tarsal Tunnel Syndrome
- Ingrown Toenails
- Arthritis (such as Gout, Rheumatoid, and Osteoarthritis)
- Flat Feet
- Injury (from stress fractures, broken toe, foot, ankle, Achilles tendon ruptures, and sprains)
- And more
Diagnosis
To figure out the cause of foot pain, podiatrists utilize several different methods. This can range from simple visual inspections and sensation tests to X-rays and MRI scans. Prior medical history, family medical history, and any recent physical traumatic events will all be taken into consideration for a proper diagnosis.
Treatment
Treatment depends upon the cause of the foot pain. Whether it is resting, staying off the foot, or having surgery; podiatrists have a number of treatment options available for foot pain.
If you have any questions, please feel free to contact our office located in New York, NY . We offer the newest diagnostic and treatment technologies for all your foot care needs.